

In this consumer-pro environment, where the emphasis is increasingly shifting towards patient-centric care and value-based models, the importance of improving patient satisfaction has become more prominent than ever.
For healthcare providers, the primary obligation has always been to deliver the highest quality of care. However, in today’s healthcare environment, this commitment extends beyond just clinical outcomes; it also encompasses the overall patient experience.
The introduction of reimbursement models that hinge on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) score is a testament to this shift
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) often, pronounced as (hcaps) is a standardized survey instrument and data collection methodology used across the United States for measuring patients’ perceptions of their hospital experience. It was officially implemented in October 2006 and first reported in March 2008.
Developed by the Centers for Medicare & Medicaid Services (CMS) in partnership with the Agency for Healthcare Research and Quality (AHRQ), HCAHPS provides a national standard for collecting and publicly reporting information that allows for a comparison of hospitals from the patient’s viewpoint.
HCAHPS scores, derived from the Hospital Consumer Assessment of Healthcare Providers and Systems survey, serve as a critical benchmark in evaluating the quality of patient care in hospitals. This survey, comprehensive in nature, includes 29 items that collectively measure essential aspects of a patient’s recent hospital experience. These items are meticulously designed to cover a wide range of factors that significantly impact patient satisfaction and perception of care received.
Of the 29 items in the survey, 19 are core questions focusing on crucial aspects of the hospital experience. These include communication with nurses and doctors, the responsiveness of hospital staff, communication about medicines, information provided at discharge, care transition, the cleanliness and quietness of the hospital environment, the patient’s overall rating of the hospital, and whether the patient would recommend the hospital to others. These questions are pivotal in understanding how patients perceive their interactions with healthcare providers and the hospital environment.
Additionally, the survey contains three items that guide patients through the questionnaire, ensuring they answer only the questions relevant to their experience. There are also five items specifically designed to adjust for the varying mix of patients across different hospitals. This adjustment is crucial to ensure that comparisons between hospitals are fair and take into account the diversity of patient populations.
Lastly, two items are included to support reports mandated by Congress, highlighting the survey’s role not only in patient care assessment but also in informing healthcare policy and regulation.
The HCAHPS survey helps compare hospitals in a fair way by measuring what patients think about their care. This comparison makes it easier for patients to see which hospitals do well.
Hospitals use these scores to understand what patients feel and where they need to get better. Sharing these scores with the public means hospitals have to work hard to keep improving.
The government also uses these scores to decide how much money hospitals get. Hospitals with higher scores get more money, so they really want to make sure their patients are happy.
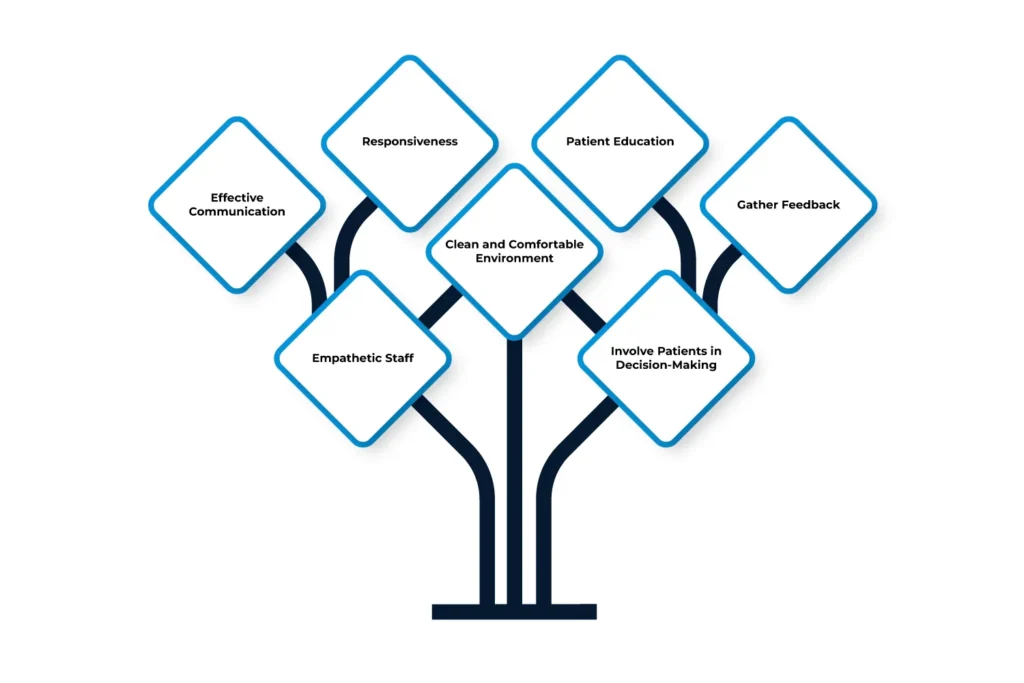
Improving patient satisfaction in hospitals is crucial for providing quality healthcare and maintaining a good reputation. Here are some effective ways hospitals can enhance patient satisfaction:
Effective Communication: Ensure clear and compassionate communication between healthcare providers and patients. Patients should feel heard and understood, and their questions and concerns should be addressed promptly.
Empathetic Staff: Train staff to be empathetic and patient-focused. A kind and understanding approach can significantly improve a patient’s experience.
Responsiveness: Be quick in responding to patient needs. Whether it’s answering a call bell or addressing pain management, timely responses make patients feel valued and cared for.
Clean and Comfortable Environment: Keep the hospital environment clean and comfortable. A tidy and quiet setting contributes to patient wellbeing.
Patient Education: Provide clear and thorough education about treatments, medications, and post-discharge care. Patients who are well-informed are more likely to be satisfied with their care.
Involve Patients in Decision-Making: Include patients in decisions about their treatment. When patients are part of the decision-making process, they are more likely to be satisfied with their care.
Gather Feedback: Regularly collect and analyze patient feedback. Understanding patient experiences and making necessary changes based on their feedback is key to improving satisfaction.
Improving patient satisfaction is essential for healthcare providers, particularly in the context of the HCAHPS survey. Remote Patient Monitoring (RPM) and Telehealth services can play a significant role in enhancing various aspects of patient care, as outlined by the HCAHPS survey.
Achieving High Scores: Patients tend to give higher ratings to doctors who effectively communicate their treatment plans, show empathy, and educate patients about their treatment. Clear communication helps in building trust, which is crucial for patient satisfaction.
Role of Telehealth: Telehealth services facilitate more frequent and flexible communication between patients and doctors. Through virtual consultations, patients can receive detailed explanations of their treatment plans and have their queries addressed promptly, which can lead to higher satisfaction scores.
Enhancing Nurse-Patient Interaction: Effective communication with nurses is vital for patient satisfaction. Nurses who are attentive, empathetic, and informative can significantly improve the patient’s hospital experience.
Telehealth Impact: Telehealth can augment this by enabling nurses to provide timely follow-ups and health education remotely, ensuring continuous patient engagement and support.
Improving Responsiveness: Prompt responses to patient needs are a key factor in patient satisfaction. Hospitals need to ensure that staff are available and responsive to patient queries and concerns.
RPM’s Contribution: RPM systems can alert hospital staff to changes in a patient’s condition, enabling quicker response times and more proactive care.
Importance of Medication Management: Educating patients about their medications and ensuring adherence is critical for both recovery and satisfaction.
Telehealth and RPM Benefits: These technologies can facilitate medication reminders, education about drug interactions, and monitoring of medication adherence, contributing to better patient outcomes and satisfaction.
Clarity in Discharge Planning: Comprehensive discharge information, including follow-up care and medication management, is crucial for patient understanding and compliance.
Telehealth for Post-Discharge Support: Telehealth services can provide virtual follow-up appointments and additional information, helping patients feel supported even after they leave the hospital
Seamless Care Transitions: Smooth transitions from hospital to home care or other facilities are essential for maintaining patient health and satisfaction.
RPM’s Role in Transition: RPM can offer continuous monitoring and support during this transition, ensuring that patients receive the necessary care and guidance, which reflects positively in HCAHPS scores.
Global Touch LLC’s telehealth services make it easier for hospitals to make patients happy. Their tools help doctors and nurses talk better with patients and keep an eye on their health even after they leave the hospital. By using these modern ways, hospitals can do a better job in all the areas that the HCAHPS survey looks at. This means patients will be more satisfied with their care, and hospitals can get better scores.
Talk to an Expert Now