

The challenge of reducing healthcare costs is an ongoing battle for every healthcare provider. In today’s healthcare landscape, reducing costs while maintaining high-quality patient care is a paramount concern. How to reduce healthcare costs? This question resonates throughout the healthcare industry. The rise of telehealth and Remote Patient Monitoring (RPM) offers a beacon of hope.
In this blog, we explore telehealth and remote patient monitoring (RPM) as part of the solution. We will explore the practical ways in which telehealth and RPM can be integrated into healthcare practices to achieve cost efficiency without sacrificing the quality of patient care.
In the current healthcare landscape, where cost efficiency is as crucial as quality care, telehealth has emerged as a vital tool for cost reduction. This innovative approach to healthcare delivery is not just a convenience; it’s a game-changer in managing healthcare expenses.
Telehealth refers to the use of electronic information and telecommunication technologies to support long-distance clinical healthcare, patient and professional health-related education, and public health administration. Let’s discuss several ways as how does telehealth reduce costs.
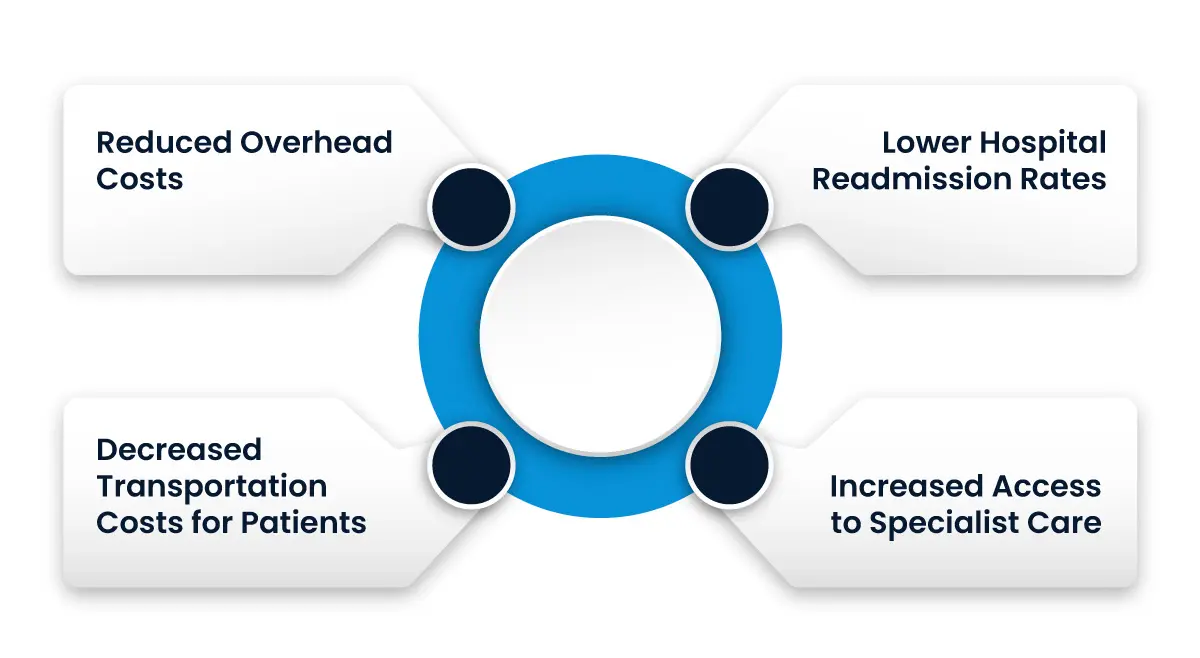
Reduced Overhead Costs: Telehealth diminishes the need for physical space and resources typically required for in-person consultations. By conducting appointments virtually, healthcare providers can save on rent, utilities, and administrative costs associated with maintaining a physical office.
Decreased Transportation Costs for Patients: Telehealth eliminates the need for patients to travel to a healthcare facility for routine consultations, follow-ups, and some types of therapy. This not only saves on transportation costs but also reduces the time and productivity lost in travel.
Lower Hospital Readmission Rates: Through telehealth, continuous monitoring of patients with chronic conditions or those recently discharged from hospitals is possible. This leads to earlier detection of potential complications, reducing the frequency of readmissions, which are often costly.
Increased Access to Specialist Care: Telehealth allows patients in remote or underserved areas to consult with specialists without incurring travel costs. This not only saves money but also ensures timely medical intervention, potentially avoiding more severe health complications that are costlier to treat.
While telehealth is a powerful tool for cost reduction, its implementation comes with challenges. These include ensuring patient and provider comfort with technology, maintaining patient privacy, and navigating reimbursement policies. To address these, healthcare providers can:
Invest in user-friendly technology and provide training for staff and patients.
Ensure compliance with health data protection laws to safeguard patient privacy.
Stay informed about telehealth reimbursement policies and insurance coverage changes.
Remote Patient Monitoring (RPM) is revolutionizing the way healthcare providers manage costs while delivering quality care. This innovative approach utilizes digital technology to monitor patients remotely, offering a seamless blend of convenience, efficiency, and cost-effectiveness.
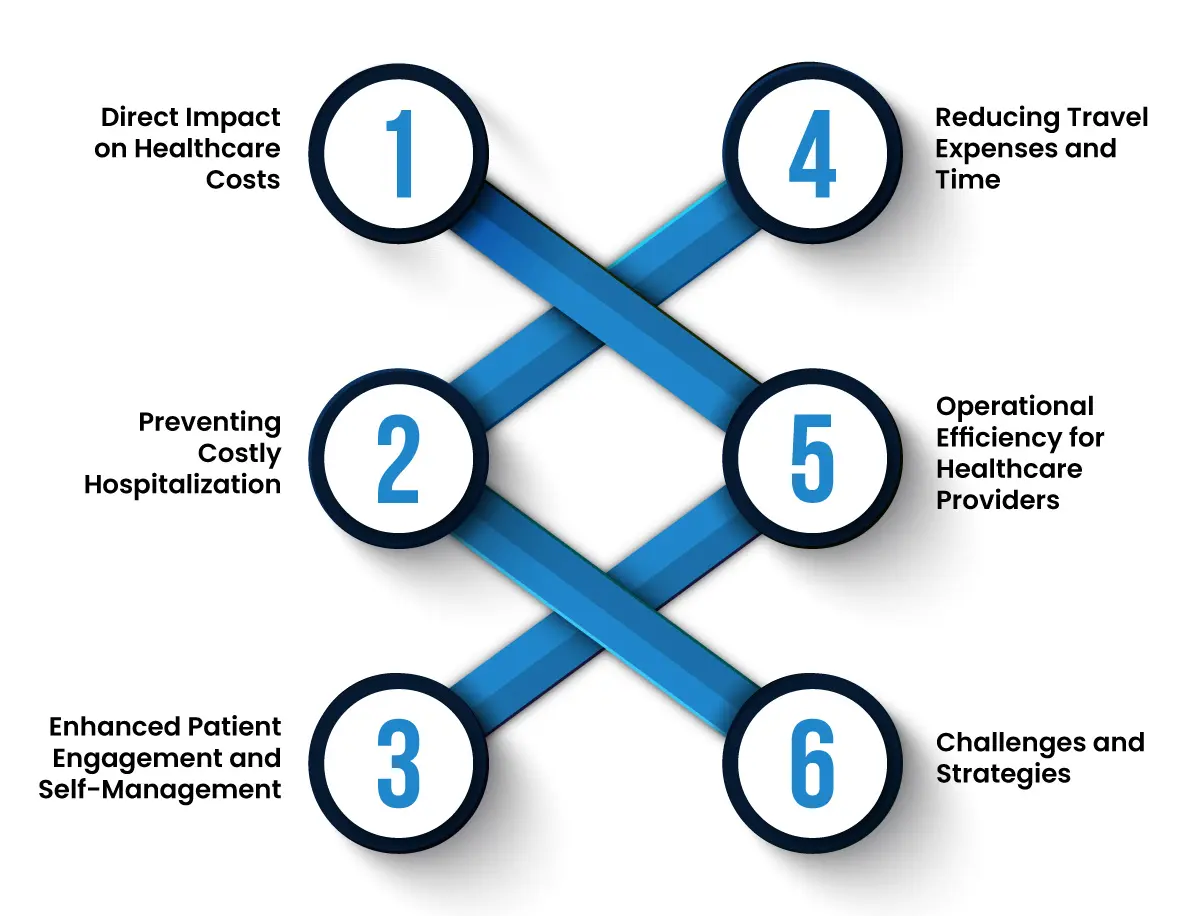
Direct Impact on Healthcare Costs:
RPM significantly lowers healthcare costs by reducing the need for frequent in-person visits. For patients with chronic conditions or those in post-operative care, RPM provides continuous monitoring, allowing healthcare providers to manage their patients’ health effectively from a distance. This not only saves on the costs associated with physical consultations but also reduces the strain on healthcare facilities.
Preventing Costly Hospitalizations:
One of the most significant advantages of RPM is its ability to prevent severe health episodes that lead to expensive hospital stays. By continuously tracking vital signs and other health metrics, RPM enables early detection of potential health issues. Timely interventions can prevent conditions from worsening, thereby avoiding costly emergency room visits and hospitalizations.
Enhanced Patient Engagement and Self-Management:
RPM empowers patients to take an active role in their health management. With real-time data at their fingertips, patients are more inclined to adhere to their treatment plans and make healthier lifestyle choices. This proactive approach to health management can lead to better overall health outcomes and reduced long-term healthcare costs.
Reducing Travel Expenses and Time:
For patients living in remote areas, or for those with mobility issues, traveling to healthcare facilities can be both challenging and expensive. RPM eliminates the need for regular travel to doctors’ offices, saving patients both time and money.
Operational Efficiency for Healthcare Providers:
Healthcare providers benefit from the operational efficiencies brought by RPM. It allows for better resource allocation and can reduce the burden on healthcare staff. By focusing on patients who need immediate attention, providers can optimize their schedules and reduce operational costs.
Challenges and Strategies:
Despite its benefits, RPM implementation faces challenges, such as ensuring patient and provider comfort with the technology, data security, and integration into existing healthcare systems. Addressing these challenges involves investing in secure and user-friendly platforms, training for both staff and patients, and staying updated with healthcare IT developments.
Reducing healthcare costs while enhancing patient outcomes is a major challenge facing the healthcare industry today. The integration of telehealth and Remote Patient Monitoring (RPM) presents an effective strategy for achieving this. Here’s how these technologies are reshaping cost management in healthcare:
Hospital readmissions not only incur high costs but also reflect on the quality of patient care. Telehealth and RPM stand out as key solutions. By closely monitoring patients at risk of readmission and offering virtual care solutions, healthcare providers can significantly reduce these occurrences. Enhanced patient education about their conditions and clear post-discharge instructions further contribute to this reduction. The bonus? Improved patient outcomes can lead to higher Medicare reimbursement rates and bolster the facility’s reputation.
Staff shortages and burnout can adversely affect patient care, leading to longer hospital stays and increased readmissions. Telehealth and RPM can alleviate this burden. Implementing remote care models, such as ‘Hospital at Home,’ not only eases the load on healthcare staff but also enhances patient outcomes. This shift leads to more efficient care delivery and a reduction in overall healthcare costs for both patients and providers.
Continuous care is vital, especially for patients with chronic conditions or those recently discharged. Telehealth and RPM facilitate this by optimizing healthcare professionals’ time and improving communication with patients. Features like remote biometric monitoring, virtual visits, symptom surveys, medication reminders, and patient education help reduce unnecessary hospital visits and minimize the likelihood of readmissions.
Accurately leveraging RPM can open up consistent revenue streams for healthcare facilities. However, navigating the reimbursement landscape, especially for newcomers, can be complex. Enlisting the help of specialists in telehealth and RPM reimbursements can ensure that you not only stay on top of the reimbursement process but also continue to deliver high-quality care. Resources like the HRS Reimbursement Calculator and guides on the HRS Blog can be invaluable in this process.
Value-based care focuses on quality and patient outcomes to keep costs down for both payers and providers. While there are barriers to fully implementing this model, RPM addresses many of these challenges. It enhances the ability to provide value-based care, thus reducing long-term operational costs. As this care model gains prominence, adopting telehealth and RPM can be a critical step in reinforcing value-based care within your facility.
By harnessing the power of telehealth and RPM, healthcare providers can make significant strides in reducing costs while maintaining, or even improving, the quality of care. This approach not only benefits patients but also enhances the operational efficiency and financial health of healthcare facilities.
In conclusion, the integration of telehealth and Remote Patient Monitoring (RPM) offers a clear answer to the pressing question: how can healthcare costs be reduced? By embracing these technologies, healthcare providers can not only achieve substantial cost savings but also elevate the standard of patient care. As we continue to navigate the complexities of healthcare economics, it’s evident that telehealth and RPM are not just tools of convenience but essential components in building a more cost-effective and patient-centric healthcare system.
Talk to an Expert Now