
12 Foods You Should Eat Every Day to Combat Common Health Concerns
12 Foods You Should Eat Every Day to Combat Common Health Concerns We all have a complicated relationship with food. Sometimes, it’s a source of
When we talk about provider intercommunication, it’s vital to understand the role played by SOAP notes. The realm of documentation might feel like an unending maze when handling SOAP notes, but it doesn’t have to be. In this blog post, we’ll break down everything providers need to know about SOAP notes in order to streamline their communication processes.
SOAP note is considered one of the most common and widely used documentation methods in healthcare settings. It is a structured format that healthcare providers use to organize patient information in a clear and concise manner. Most of the modern-day healthcare elements are a part of the SOAP note, including modern-day EHR systems, HHS, and CMS.
SOAP is an acronym for Subjective, Objective, Assessment, and Plan. Each component plays a crucial role in creating a comprehensive SOAP note. Understanding the soap notes meaning reveals it as a well-structured and organized method of documenting the history and progress of patients during treatment. Utilizing SOAP notes facilitates the delivery of high-quality care and ensures effective communication between healthcare providers.
The SOAP note format was first introduced as a teaching tool in the early 1960s at the University of Vermont College of Medicine. It was developed by Dr. Lawrence Weed, a physician and medical educator, who aimed to address the deficiencies he observed in medical documentation and diagnosis.
Dr. Weed believed that traditional narrative-style charting lacked structure and consistency, making it difficult for healthcare providers to communicate and analyze patient information effectively.
The SOAP acronym, which stands for Subjective, Objective, Assessment, and Plan, is a widely used and standardized method of organizing and documenting patient information in the medical field. Each letter in the SOAP medical abbreviation represents a specific section of the patient’s medical record or clinical note. Here’s a detailed explanation of each component:
This is the first section of the SOAP note and focuses on gathering information that is subjective or based on the patient’s perspective. It typically includes:
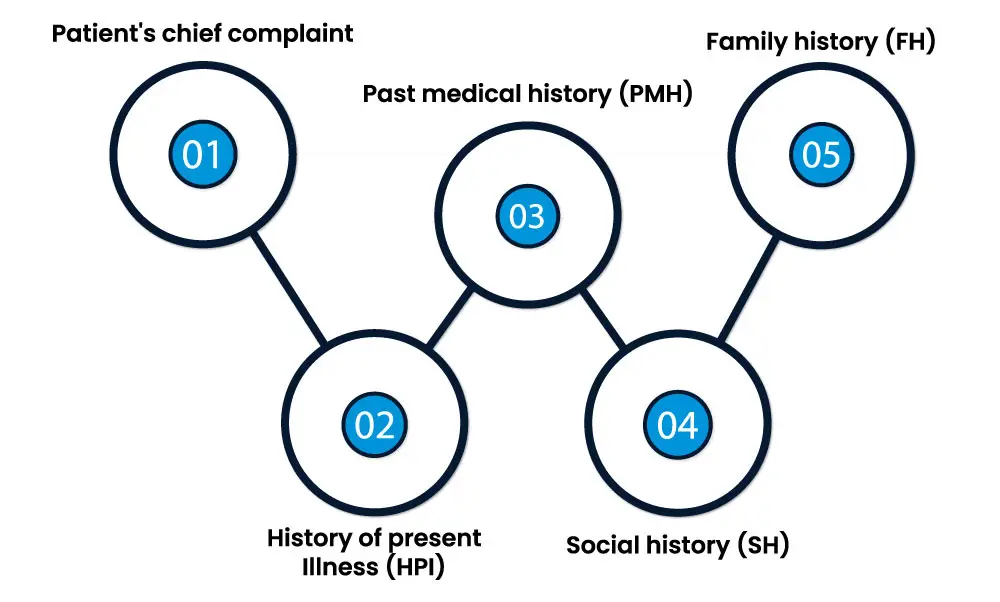
Patient’s chief complaint: The primary reason the patient sought medical attention.
History of present illness (HPI): A detailed description of the current symptoms, including their onset, duration, severity, and any exacerbating or alleviating factors.
Past medical history (PMH): Relevant information about the patient’s medical history, including previous illnesses, surgeries, and chronic conditions.
Social history (SH): Information about the patient’s lifestyle, habits, and social factors that may impact their health, such as smoking, alcohol use, and living conditions.
Family history (FH): Any significant medical conditions or diseases that run in the patient’s family.
The objective section contains data that is measurable, quantifiable, and based on clinical observations, diagnostic tests, and physical examinations. This section typically includes:
Vital signs: Essential measurements like blood pressure, heart rate, respiratory rate, and body temperature.
Physical examination findings: Detailed descriptions of the patient’s physical condition, including examination of body systems, such as the cardiovascular, respiratory, gastrointestinal, and musculoskeletal systems.
Laboratory and diagnostic test results: Objective data from tests like blood work, imaging studies (e.g., X-rays or MRIs), and electrocardiograms (ECGs).
Any other relevant objective data: This can include measurements like height, weight, and body mass index (BMI).
The assessment section involves the healthcare provider’s professional judgment and analysis of the patient’s condition. It includes:
Diagnosis or differential diagnosis: The healthcare provider’s assessment of the patient’s condition, which may include a primary diagnosis, possible alternative diagnoses (differential diagnoses), and any uncertainties.
Discussion of the patient’s progress: A summary of the patient’s response to previous treatments and interventions.
Identification of any complications or comorbidities
The plan section outlines the healthcare provider’s recommended course of action for the patient’s care. It typically includes:
Treatment plan: Details of the treatment approach, including medications prescribed, therapies, procedures, or surgeries planned.
Follow-up appointments: Scheduling and recommendations for future appointments, tests, or evaluations.
Patient education: Information provided to the patient about their condition, treatment options, and lifestyle modifications.
Any additional considerations: This can encompass referrals to specialists, consultations, and discussions of advanced care directives or other relevant aspects of patient care.
The SOAP acronym serves as a structured framework for documenting patient information, facilitating clear and organized communication among healthcare providers, and ensuring that all essential aspects of the patient’s care are documented comprehensively. It is a fundamental tool for healthcare professionals in various medical specialties and clinical settings, contributing to effective patient care and continuity of care.
Begin your SOAP note by providing essential patient information, such as their name, age, and the date and time of the encounter. This sets the context for the note and ensures proper documentation.
In the Subjective (S) section, capture the patient’s main complaint and any symptoms they report. It’s crucial to gather information about:
Additionally, include relevant details from the patient’s past medical history, social history, and family history that are pertinent to the current complaint.
Move on to the Objective (O) section, where you record objective data acquired through physical examinations, diagnostic tests, and observations. Vital signs like blood pressure and heart rate should be documented.
Provide details of your physical examination findings, highlighting any clinical abnormalities or notable signs. Incorporate laboratory results, radiological findings, and any other diagnostic data relevant to the patient’s condition.
In the Assessment (A) section, offer your professional assessment or diagnosis based on the information collected in the subjective and objective sections. Clearly state the primary diagnosis, any alternative diagnoses (differential diagnoses), and note any uncertainty or the need for further evaluation. Summarize the patient’s overall condition and highlight any relevant comorbidities or complications.
Next, in the Plan (P) section, outline the proposed plan for the patient’s treatment and ongoing care. Specify the treatment approach, including
If applicable, describe planned procedures, therapies, or surgeries. Schedule follow-up appointments and indicate their purpose, whether for monitoring, receiving test results, or adjusting treatment. Provide patient education, covering essential information about their condition, recommended lifestyle modifications, and potential side effects of prescribed treatments. Mention any referrals to specialists or consultations with other healthcare providers and address any additional considerations, such as advanced care directives if they apply.
Conclude your SOAP note with your name, title, and contact information. Sign and date the note to confirm its accuracy and completion. Ensure that your note complies with any legal, regulatory, or institutional documentation requirements, using clear and straightforward language while safeguarding patient confidentiality. Lastly, remember to review and update the SOAP note as necessary to reflect changes in the patient’s condition or treatment plan.
SOAP (Subjective, Objective, Assessment, Plan) notes are used by a wide range of healthcare professionals across various clinical settings.
Avoiding common mistakes when writing SOAP (Subjective, Objective, Assessment, Plan) notes is essential to ensure accurate patient documentation and effective communication among healthcare providers. Here are some common SOAP note mistakes to be mindful of:
| Mistake | Avoidance |
| Using vague language or unclear descriptions of symptoms, findings, or assessments | Use precise and specific terms to describe the patient’s condition, symptoms, and observations. |
| Failing to include relevant subjective details provided by the patient | Carefully record the patient’s chief complaint, history of present illness, and any pertinent information they share about their condition |
| Omitting critical objective information such as vital signs, physical examination findings, or diagnostic test results | Include all relevant objective data to support your assessment and treatment plan. |
| Providing a diagnosis without adequate evidence or misdiagnosing the patient’s condition | Base your diagnosis on the collected data, clinical findings, and patient history. Be transparent about diagnostic uncertainties |
| Writing illegible notes that can lead to misinterpretation or errors in patient care. | Use legible handwriting or consider electronic health records (EHRs) for documentation |
| Not adhering to the SOAP note format consistently, which can lead to confusion | Follow the SOAP format rigorously to maintain clarity and consistency in documentation |
| Failing to protect patient privacy by leaving notes accessible to unauthorized personnel. | Store and share SOAP notes securely in compliance with healthcare privacy regulations. |
(SOAP) notes offer several benefits in healthcare settings, contributing to efficient and effective patient care. Here are some of the key advantages of using SOAP notes:
Structured Documentation: SOAP notes provide a standardized and structured format for documenting patient information. This format ensures that all essential aspects of a patient’s condition, assessment, and treatment plan are consistently and comprehensively documented.
Clear Communication: The structured layout of SOAP notes promotes clear and organized communication among healthcare providers. It enables healthcare professionals to quickly understand a patient’s status, making it easier to provide continuous and coordinated care.
Comprehensive Assessment: SOAP notes encourage healthcare providers to assess patients from multiple angles, including subjective information (patient-reported symptoms), objective data (measurable findings), assessment (diagnoses or impressions), and plans (treatment strategies). This comprehensive approach enhances the accuracy of diagnoses and treatment plans.
Continuity of Care: SOAP notes facilitate continuity of care, ensuring that essential patient information is readily available to other healthcare team members. This is particularly valuable when patients are seen by multiple providers or when there is a need for care transitions.
Legal and Regulatory Compliance: SOAP notes often meet legal and regulatory requirements for healthcare documentation. Accurate and comprehensive documentation is crucial for medical billing, insurance claims, and maintaining compliance with healthcare laws.
Efficiency and Time Management: The SOAP format encourages concise and organized documentation, saving time for healthcare providers. It allows for the quick retrieval of relevant information, reducing the need to sift through lengthy narratives.
Patient Information:
Subjective (S):
The patient presents with a complaint of severe headache that started yesterday. Mr. Doe reports a throbbing headache on the left side of his head. He describes the pain as 8/10 in intensity and notes that it’s accompanied by nausea and sensitivity to light. He denies any recent head trauma or changes in vision. The patient has a history of occasional tension headaches but states that this episode feels different.
Objective (O):
Vital Signs:
Physical Examination:
Neurological examination is unremarkable. No focal deficits observed.
Pupils are equal, round, and reactive to light (PERRLA).
Diagnostic Tests:
No abnormal findings in the complete blood count (CBC) and comprehensive metabolic panel (CMP).
Normal findings on a non-contrast head CT scan, ruling out any acute intracranial abnormalities.
Assessment (A):
Mr. Doe presents with a severe headache, suggestive of a migraine with aura based on the one-sided throbbing pain, associated nausea, and photophobia. Differential diagnoses considered include tension headache and cluster headache. The patient is alert, oriented, and stable. No neurological deficits are noted.
Plan (P):
Prescribed sumatriptan 50mg orally for acute migraine relief, to be taken as needed, with a maximum of two doses within 24 hours. Advised Mr. Doe to rest in a dark, quiet room and avoid known headache triggers.
Follow-Up:
Schedule a follow-up appointment in two weeks to assess treatment response and consider long-term preventive measures. Advised the patient to keep a headache diary to track the frequency, duration, and triggers of headaches.
Patient Education:
Educated Mr. Doe on recognizing migraine triggers, lifestyle modifications, and the importance of adhering to the treatment plan. Emphasized the need to seek immediate medical attention if the headache worsens or if new symptoms develop.
Referral:
Referred Mr. Doe to a neurologist for further evaluation if there is no improvement with treatment.
Provider’s Name and Signature:
Dr. Jane Smith, MD
October 15, 2023
In conclusion, SOAP notes are a crucial aspect of patient care that offer numerous benefits to healthcare providers. The structured format, clear communication, comprehensive assessment, continuity of care, legal and regulatory compliance, efficiency and time management all contribute to improving the quality of patient care.
By understanding SOAP notes and adhering to their guidelines, healthcare professionals can ensure accurate and efficient documentation for better patient outcomes. So, next time you hear someone talking about SOAP notes, you’ll know exactly what they mean and how important they are in the healthcare industry. Remember, with great documentation comes great patient care!

12 Foods You Should Eat Every Day to Combat Common Health Concerns We all have a complicated relationship with food. Sometimes, it’s a source of

Telehealth Costs Explained: What You Need to Know A recent study revealed that 40% of Americans avoid necessary healthcare due to affordability concerns. Telehealth emerged
Talk to an Expert Now