

For years, healthcare providers have navigated the complexities of a system that often prioritizes quantity over quality, where the number of tests and treatments could overshadow the actual health outcomes. Now the the shift from the traditional fee-for-service model to value based reimbursement isn’t just a trend; it’s a transformative journey redefining how care is delivered and valued.
This innovative approach promises to align financial incentives with the quality of care, placing patient outcomes at the heart of healthcare. s a provider, embracing this change might seem daunting, but it’s a path laden with opportunities for improved patient care, enhanced provider satisfaction, and a more sustainable healthcare system.
Value-based reimbursement in healthcare is a revolutionary approach that’s reshaping how we think about and deliver medical care. In simple terms, it’s like shifting the focus from ‘how much’ to ‘how well’. Under the traditional fee-for-service model, healthcare providers are paid based on the quantity of services they deliver – think of it as a ‘more is more’ approach.
With the introduction of value-based reimbursement in healthcare reimbursement models, the focus shifts to ensuring that the treatments and services you offer genuinely benefit the patient’s health. It’s about providing the right care at the right time, in the right way.
For instance, if you’re managing a patient with diabetes, under Value-Based Reimbursement, you’re incentivized to help them control their blood sugar and avoid complications, rather than just offering more and more treatments.
For healthcare providers, understanding the differences between the Fee-For-Service model and the Value-Based Health Care model is crucial. These models fundamentally differ in how they approach patient care and compensation. To clarify these differences, here’s a concise table outlining key aspects of each model:
Aspect | Fee-For-Service Model | Value-Based Health Care Model |
Focus | Quantity of services provided | Quality and outcomes of care |
Payment Structure | Providers are paid for each service performed, like tests and procedures | Providers are financially rewarded for improving patients’ health, reducing the effects and incidences of chronic disease |
Care Approach | Emphasizes volume and frequency of visits and treatments | Emphasizes preventative care, patient outcomes, and efficient management of chronic diseases |
Provider Incentives | Incentivized to increase the number of services and procedures | Incentivized to provide effective, efficient care leading to better patient outcomes |
Patient Outcomes | Secondary to the volume of services | Central focus; the primary measure of provider performance |
Cost Implications | Can lead to increased healthcare costs due to unnecessary services | Aims to reduce unnecessary expenses, focusing on long-term cost-effectiveness and sustainability |
The Centers for Medicare & Medicaid Services (CMS) has introduced various reimbursement models to facilitate the shift towards value-based care in healthcare. These models are designed to improve patient outcomes while reducing costs by focusing on the quality rather than the quantity of care delivered. The key models implemented by CMS include:
ACOs are networks of doctors and hospitals that share financial and medical responsibility for providing coordinated care to patients. The aim is to ensure that patients, especially the chronically ill, get the right care at the right time, avoiding unnecessary duplication of services and preventing medical errors.
Providers in ACOs make joint decisions about the care of their patients, focusing on preventive measures and closely monitoring chronic conditions to improve health outcomes and lower costs.
PCMHs transform primary care into “what patients want it to be.” In this model, care is organized around the patient, leading to improved access, better preventive services, and integration of behavioral health and primary care. Emphasis is placed on the coordination of care, especially for those with complex health needs, ensuring patients receive the necessary care when and where they need it, in a manner they can understand.
This model involves making a single payment to cover services across a single episode of care, such as heart surgery or a hip replacement. It encourages healthcare providers to work together to provide more coordinated and efficient care. The payment is based on the expected costs for a clinically-defined episode of health care. Providers can earn additional payment if they reduce costs while maintaining or improving quality of care.
These programs adjust payments to hospitals under the Inpatient Prospective Payment System (IPPS) based on the quality of care they deliver. The program uses several measures of care quality, including patient experience and care efficiency. Hospitals are rewarded for delivering high-quality, efficient clinical care and for providing a high level of patient satisfaction.
Under this program, ACOs are incentivized to reduce the growth of healthcare costs while meeting performance standards on key quality measures, including patient/caregiver experience, care coordination, and patient safety. Successful ACOs that achieve cost savings against a benchmark while meeting quality standards share in the savings with Medicare.
This payment model offers providers a flat fee per patient, covering all the care the patient needs for a set period. It encourages providers to focus on keeping patients healthy and out of the hospital, as the provider bears the financial risk for the cost of services. This model drives a more holistic approach to patient care, emphasizing preventive care and careful management of chronic diseases.
Reimbursement in healthcare is crucial for several reasons.
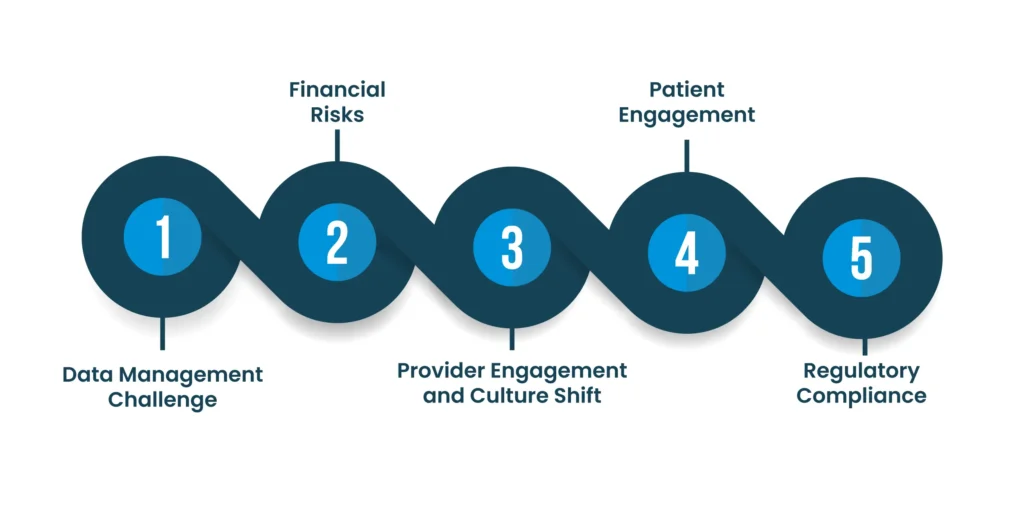
Data Management Challenge: Providers transitioning to value-based models need comprehensive data to track and improve patient outcomes. For example, a small clinic might struggle to invest in advanced data systems to monitor patient health trends and outcomes effectively, impacting their ability to make data-driven decisions.
Financial Risks: Shifting to value-based care often requires upfront investments in technology, staff training, and changes in care delivery, posing financial risks. A hospital might face reduced income initially as it moves away from fee-for-service models, where more procedures equate to higher revenues.
Provider Engagement and Culture Shift: Moving to a value-based model requires a cultural shift within the organization. For instance, a healthcare provider used to operating in a high-volume environment may resist changing their practice to focus more on patient outcomes than on the number of patients seen.
Patient Engagement: Engaging patients in their care is vital but challenging. For example, a provider might find it difficult to motivate patients to adhere to treatment plans or make lifestyle changes, which are crucial for the success of value-based care.
Regulatory Compliance: Adapting to the evolving regulations of value-based models while maintaining compliance is complex. A healthcare system might struggle to keep up with changing reimbursement rules and documentation requirements, risking penalties or reduced payments
Remote monitoring can significantly aid healthcare providers in achieving higher value-based reimbursements in several ways:
Increased Patient Engagement and Satisfaction: Continuous care through telehealth and remote patient monitoring (RPM) increases patient engagement and satisfaction. Providers can maintain regular contact with patients, offering care and advice from the comfort of the patient’s home, leading to better health outcomes and higher patient satisfaction rates.
Cost Reduction: Telehealth and RPM reduce overall healthcare costs. By minimizing the need for in-person visits, it saves on travel costs for patients and reduces the operational costs for providers. This cost-effectiveness is a key component in value-based care models.
Reduced Hospital Readmissions: One of the major advantages of remote monitoring is its effectiveness in reducing hospital readmissions. By closely monitoring patients, especially those with chronic conditions, healthcare providers can identify and address issues early, preventing the need for hospital readmissions, which is a critical metric in value-based reimbursement models.
Overall, the adoption of remote monitoring aligns with the principles of value-based care by emphasizing preventive care, patient engagement, and cost-effective treatment, ultimately contributing to higher reimbursements for providers.
In conclusion, the transition to value-based reimbursement models in healthcare represents a significant shift towards prioritizing patient outcomes and cost-effectiveness. This shift challenges providers to adapt in certain areas.
Remote monitoring technologies offer a strategic advantage in this transition These innovations align with the core objectives of value-based care, potentially leading to higher reimbursements and improved healthcare delivery.
For healthcare providers seeking to navigate these changes effectively and learn more about implementing value-based reimbursement models, discussing strategies with a reimbursement specialist at Global Touch LLC can provide valuable insights and guidance.
Talk to an Expert Now