

In the United States, the ticking of the clock holds a more ominous significance for heart health, with a heart attack striking approximately every 40 seconds. These events, ranging from the dramatically symptomatic to the stealthily silent, underscore the unpredictability and danger lurking within our own rhythms. Imagine, then, having a window into the very essence of your heart’s function, particularly in those crucial seconds when the risk of a heart attack looms large.
This window isn’t just a figment of imagination but a tangible reality made possible by the EKG—a tool that peers into the heart’s electrical activities to reveal the truth of its wellbeing. But can this device, with its modest setup of wires and patches, truly detect the onset of a heart attack, offering a beacon of hope and timely intervention?
Let’s explore together the significance of the EKG in the medical field, how it functions, and why it’s often the first tool used in the fight against heart attacks.
An EKG (electrocardiogram) is a test that measures the electrical activity of the heart. This activity is crucial because it helps the heart to contract and pump blood throughout the body. The EKG translates this electrical activity into line tracings on paper, with spikes and dips known as waves.
Here’s a simple breakdown of what the EKG shows:
During an EKG, small electrode patches are attached to the skin on your chest, arms, and legs. These electrodes detect the tiny electrical changes on the skin that arise from the heart muscle’s electrophysiologic pattern of depolarizing during each heartbeat. It’s a quick, non-invasive, and painless test that provides valuable information about your heart.
Yes, an EKG (electrocardiogram) can detect a heart attack. It does so by measuring the heart’s electrical activity, which can show if a part of the heart is not receiving enough blood flow, a common issue during a heart attack. An EKG can identify abnormal patterns that suggest the heart muscle is under stress or has been damaged, which are key indicators of a heart attack.
Here’s how an EKG can signal a heart attack:
Ischemia refers to a reduced blood flow to the heart muscle, starving it of oxygen. An EKG can show signs of ischemia through specific changes in the ST segment and T wave, suggesting that parts of the heart are not receiving enough blood.
An EKG can detect arrhythmias (abnormal heart rhythms), which may indicate underlying heart conditions that could lead to a heart attack. Some arrhythmias increase the risk of forming blood clots in the heart, which can then lead to a heart attack.
A heart beating too fast, too slow, or irregularly can be a sign of stress on the heart or potential blockages in the heart’s electrical pathways, possibly leading up to a heart attack.
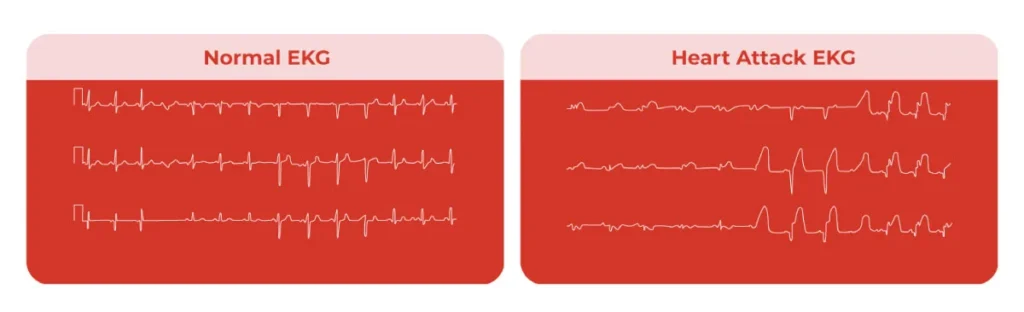
The differences between a heart attack EKG and a normal EKG are primarily seen in the patterns and shapes of the waves and segments on the EKG readout, which reflect the heart’s electrical activity. These differences indicate how the heart’s muscle cells are functioning and can show if a part of the heart is not getting enough blood (ischemia) or has been damaged by a heart attack.
A normal EKG has a specific pattern of P waves, QRS complex, T waves, and sometimes U waves that occur in a regular rhythm and sequence:
Yes, an EKG (electrocardiogram) can often detect signs of a previous heart attack. Certain features on the EKG can indicate that a portion of the heart muscle has been damaged or scarred, suggesting a heart attack occurred in the past. These signs can be permanent or very long-lasting on the EKG readings, providing clues about historical events in the heart’s health.
The accuracy of an EKG in detecting a previous heart attack can be influenced by several factors:
Larger heart attacks that cause more extensive damage are more likely to be detected on an EKG because they produce more pronounced changes in the electrical activity of the heart.
The location of the heart attack within the heart muscle can affect detectability. Some areas might produce clearer EKG evidence than others.
Immediately after a heart attack, certain EKG signs are more pronounced. Over time, some of these signs might become less apparent, though pathological Q waves typically remain.
Other conditions affecting the heart, such as hypertrophy (thickening of the heart muscle) or other types of heart disease, can complicate the interpretation of an EKG.
While an EKG is a valuable tool for detecting a previous heart attack, it is not infallible. Some people who have had a minor heart attack may not show permanent changes on an EKG. Additionally, not all damage to the heart results in the specific EKG changes mentioned above.
For these reasons, EKG results are often combined with other tests and the patient’s clinical history for a more accurate assessment. These can include echocardiograms, MRI scans, stress tests, and blood tests for cardiac biomarkers. Together, these tools provide a more comprehensive view of the heart’s health and history.
Silent heart attacks, also known as silent myocardial infarctions, occur when the blood supply to a part of the heart muscle is severely reduced or blocked, causing damage to the heart muscle, much like a regular heart attack. However, the key difference is that silent heart attacks happen without the typical symptoms associated with a heart attack, or the symptoms are so mild that they are often mistaken for less serious health issues.
In wrapping up our exploration of the invaluable role EKGs play in heart health, it’s evident that while they are pivotal in identifying past heart attacks through the detection of electrical activity abnormalities, their effectiveness is significantly enhanced when paired with other diagnostic tools. The synergy of EKG results with blood tests and imaging techniques is crucial in minimizing the risk of misdiagnosis, providing a more comprehensive picture of your heart’s condition.
If you suspect you’ve experienced a heart attack, the importance of immediate medical intervention cannot be overstressed. Prompt access to treatment can drastically improve your prognosis, underscoring the need for awareness and timely action in matters of the heart.
Talk to an Expert Now