

Hospital readmissions are not only disruptive and stressful for patients but also costly for the healthcare system. According to the Agency for Healthcare Research and Quality (AHRQ), hospital readmission rates are as high as 14%, with each readmission costing an average of $15,200.
What if there were a way to keep patients healthy and at home after they’ve been discharged, reducing the chances they’d need to return to the hospital? That’s where telehealth and Remote Patient Monitoring (RPM) step in.
These innovative tools are changing the game in healthcare, providing a bridge between patients and their care teams, and ultimately helping to lower hospital readmissions. Let’s explore how this powerful duo works and the significant impact it’s having on patient care.
The Hospital Readmission Reduction Program (HRRP), established under the Affordable Care Act, plays a crucial role in addressing hospital readmissions. This program encourages hospitals to improve the quality of care transitions and reduce preventable readmissions by financially penalizing hospitals with excessive readmissions for specific conditions.
The HRRP’s focus on reducing readmissions has led hospitals to:
Prioritize discharge planning:
Hospitals now put more emphasis on ensuring that patients understand their discharge instructions, medications, and follow-up care.
Improve care coordination:
Better communication and collaboration between hospitals, primary care providers, and specialists help ensure patients receive the necessary care after discharge.
Expand the use of telehealth and RPM:
Many hospitals have embraced telehealth and RPM technologies to improve care transitions and monitor patients remotely.
The HRRP has incentivized hospitals to implement strategies that improve patient care and reduce readmissions. By integrating telehealth and RPM into their post-discharge plans, hospitals can further enhance the quality of care transitions and ensure patients receive the support they need to stay healthy at home.
Virtual care offers several effective strategies to keep patients healthy at home and avoid unnecessary return trips to the hospital. By leveraging technology to connect patients and healthcare providers, telehealth empowers patients to participate in their care actively and allows healthcare professionals to monitor their progress remotely.
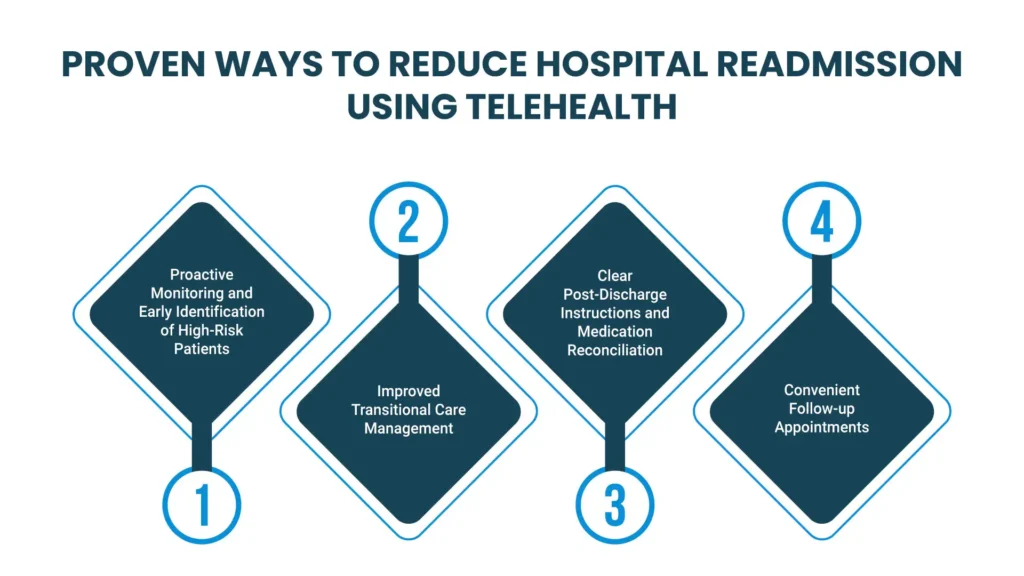
Telehealth enables healthcare providers to closely monitor patients who are at higher risk of readmission due to chronic conditions, recent surgeries, or complex medical needs. By utilizing remote patient monitoring (RPM) devices and virtual check-ins, providers can track vital signs, symptoms, and medication adherence in real-time.
This data allows for early detection of warning signs, such as changes in blood pressure, oxygen levels, or weight, that could indicate a potential decline in health. With timely intervention, healthcare professionals can address these issues before they escalate and lead to readmission.
For example, a patient with congestive heart failure might be equipped with a weight scale and blood pressure monitor that transmit readings to their healthcare team daily. If the patient’s weight suddenly increases, a sign of fluid retention, the healthcare team can quickly adjust medications or schedule a virtual appointment to assess the situation and prevent a potential trip to the hospital.
Telehealth can facilitate seamless communication and coordination between healthcare providers during the critical transition period when a patient is discharged from the hospital. Through virtual consultations and shared electronic health records, hospital teams can effectively communicate discharge instructions, medication plans, and follow-up care recommendations to primary care physicians, specialists, and home health providers. This ensures continuity of care, reduces the risk of miscommunication or errors, and empowers the patient’s care team to manage their health during the vulnerable post-discharge period proactively.
For instance, a patient with diabetes might have a virtual meeting with their primary care physician shortly after discharge. During this meeting, the hospital team can discuss the patient’s current condition, medications, and any specific concerns. The primary care physician can then seamlessly schedule follow-up appointments, order lab tests, or make medication adjustments as needed. This streamlined communication ensures that the patient receives comprehensive and coordinated care, reducing the likelihood of complications or readmission.
Inadequate post-discharge instructions and medication errors are significant contributors to hospital readmissions. Misunderstandings about medications, follow-up care, or self-care routines can lead to complications, setbacks, and ultimately, a return trip to the hospital. Telehealth offers a solution to this challenge by enhancing communication and ensuring patients are well-informed and prepared for their recovery at home.
Telehealth offers several advantages in this area:
For example, a patient discharged after a heart attack might receive a virtual visit from a nurse who demonstrates the proper use of a blood pressure monitor and explains how to recognize and respond to warning signs. Additionally, the nurse can review the patient’s medication list, ensuring there are no conflicts or misunderstandings. This level of personalized attention and clear communication can significantly reduce the likelihood of complications that could necessitate a return to the hospital.
Telehealth eliminates the need for patients to travel to the hospital or clinic for routine follow-up appointments. This is especially beneficial for individuals with limited mobility, transportation challenges, or those residing in rural areas.
Virtual follow-up appointments allow healthcare providers to assess a patient’s progress, address any concerns, and make necessary adjustments to their treatment plan from the comfort of their own home. This accessibility not only improves patient satisfaction but also encourages greater adherence to follow-up care, leading to earlier detection of potential issues and timely intervention to prevent readmissions.
For example, a patient recovering from surgery might have a virtual follow-up appointment with their surgeon to discuss their healing progress, pain management, and any potential complications. The surgeon can visually assess the surgical site, answer any questions the patient may have, and provide reassurance or additional guidance as needed. This convenience and ease of access to follow-up care help patients stay engaged in their recovery and prevent any potential setbacks that could lead to readmission.
Global Touch LLC’s Remote Patient Monitoring (RPM) solutions are designed to empower healthcare providers and patients alike in the fight against hospital readmissions. By providing the tools and technology necessary for proactive monitoring, timely intervention, and seamless communication, Global Touch LLC enables healthcare teams to deliver personalized, patient-centered care that keeps individuals healthy at home and out of the hospital.
Our comprehensive platform offers real-time data tracking, customizable alerts, and intuitive interfaces, allowing providers to identify and address potential issues before they escalate. With Global Touch LLC’s RPM solutions, reducing hospital readmissions becomes a reality, leading to improved patient outcomes, reduced healthcare costs, and a more efficient healthcare system.
Talk to an Expert Now