
8 Most Common Remote Patient Monitoring Devices
Healthcare delivery has taken a remarkable shift since the introduction of remote patient monitoring devices. With an increase in telehealth services during the pandemic era,

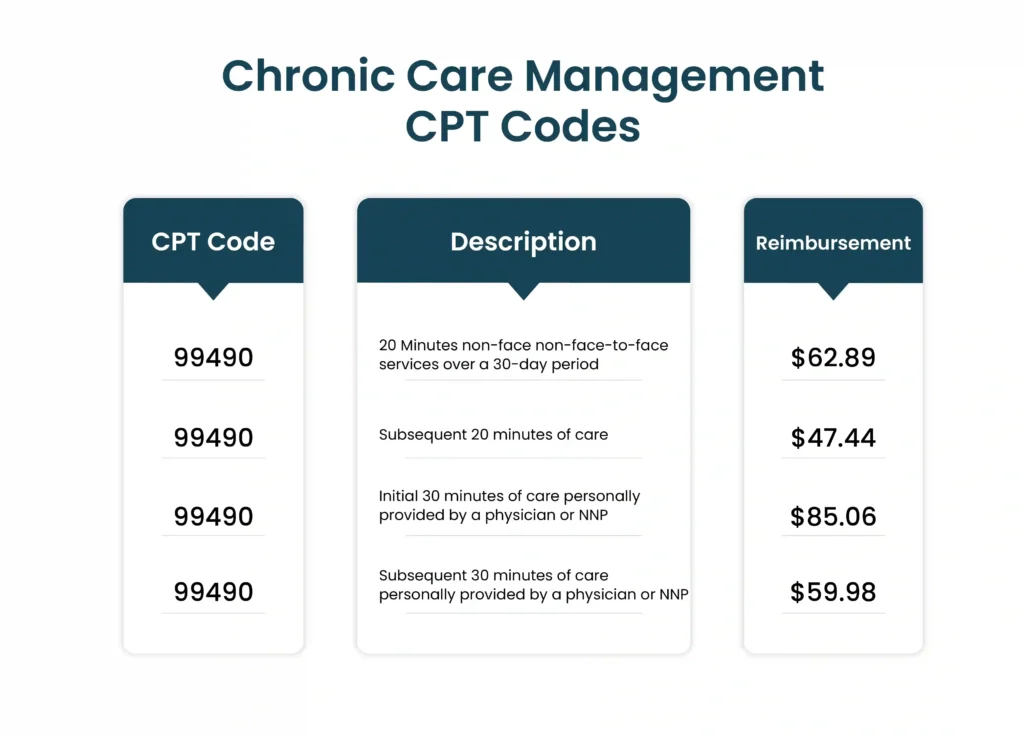
When billing for chronic care management services, it is crucial to know which Chronic Care Management CPT codes are appropriate to use. CMS unbundled CCM services, recognizing their importance in healthcare for individuals with chronic conditions, resulting in separate reimbursement for these services. This knowledge is essential for accurate billing and proper reimbursement.
In this blog guide, we are going to discuss the CPT codes used for chronic care management and explain each code’s details, including the services provided and their corresponding reimbursement rates.
Chronic Care Management (CCM) refers to the non-face-to-face services provided to Medicare beneficiaries with multiple chronic conditions. These services are designed to improve patient outcomes by providing ongoing support, coordination, and management of care. CCM services are typically provided by a physician or qualified healthcare professional (QHP) and involve creating a comprehensive care plan for the patient, regular check-ins, medication management, and coordination with other providers involved in the patient’s care.
Chronic Care Management (CCM) services encompass a range of healthcare activities designed to improve the care and management of patients with multiple chronic conditions. These services are crucial for enhancing the quality of life for patients and reducing healthcare costs through more effective management. Let’s break down what’s typically included in CCM services:
Step 1: Verify Eligibility and Obtain Consent
Before you begin, it’s crucial to verify that your patients are eligible for CCM services. Eligibility typically involves having multiple chronic conditions expected to last at least 12 months or until the end of life. Once eligibility is confirmed, obtain written or verbal consent from the patient, documenting their agreement to receive CCM services and acknowledging their understanding of any co-payments or deductibles.
Step 2: Document Comprehensive Care Planning
A comprehensive care plan is a foundational element of CCM. Ensure that you document all aspects of this plan, including the patient’s health problems, expected outcomes, measurable goals, symptom management, planned interventions, and a list of the healthcare providers involved in their care.
Step 3: Track Time Spent on CCM Services
Accurate time tracking is essential for CCM billing. Document the amount of time spent on non-face-to-face services provided to the patient each month. This includes time spent coordinating care, managing medications, and other activities related to the patient’s care plan.
Step 4: Use Correct CPT Codes
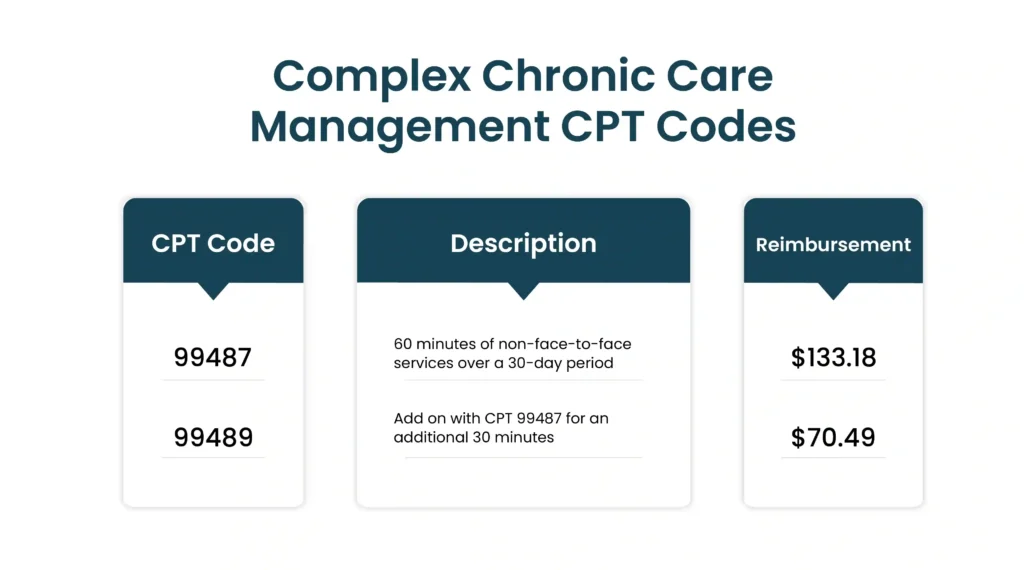
Billing for CCM services involves specific Current Procedural Terminology (CPT) codes. The main codes include 99490, 99487, 99489, and others, each representing different levels of complexity and time spent on care management. Ensure you use the appropriate code that reflects the services provided.
Step 5: Provide 24/7 Access to Care
Part of billing for CCM services involves providing patients with 24/7 access to healthcare professionals. This should be documented as part of the service, as it’s a requirement for CCM billing.
Step 6: Ensure Compliance with Medicare and Other Payers
Familiarize yourself with the specific requirements of Medicare and other insurance payers for CCM billing. This includes understanding the documentation requirements, billing procedures, and any updates to policies and procedures.
Step 7: Submit Claims in a Timely Manner
Submit your claims in a timely manner to ensure prompt payment. Make sure all the required documentation is included with your claim to avoid delays or denials.
Step 8: Monitor and Follow Up on Claims
After submitting your claims, monitor them for any updates. If there are denials or queries, respond to them promptly. Regular follow-up on the status of your claims is essential to ensure that you are compensated for the services provided.
CPT Code 99437 serves as an add-on code to CPT Code 99491 when healthcare providers require extra time beyond the initial 30 minutes of face-to-face care covered by CPT Code 99491.
CPT Code 99487 is designated for complex chronic care services. Providers are required to allocate a minimum of 60 minutes of non-face-to-face clinical staff time for enrollees with multiple (two or more) chronic conditions expected to last at least 12 months or until the patient’s death.
CPT Code 99489 is used in conjunction with CPT Code 99487 to bill for an additional 30 minutes of non-face-to-face service. Providers may use this code when the complexity of the patient’s chronic conditions and care management necessitates an extra 30 minutes beyond what is covered by CPT Code 99487.
Effective chronic care management is crucial for improving patient outcomes, reducing hospitalizations and emergency room visits, and enhancing overall quality of life. Familiarizing yourself with the necessary steps for billing CCM services, understanding the appropriate CPT codes to use, and remaining compliant with Medicare and other insurance payers’ requirements will ensure a smooth reimbursement process.

Healthcare delivery has taken a remarkable shift since the introduction of remote patient monitoring devices. With an increase in telehealth services during the pandemic era,

What Qualifies a Patient for Skilled Nursing Care? Witnessing a family member or friend’s age can be an emotionally charged experience. As the hands of
Talk to an Expert Now