
What is Chronic Care Management?
What is Chronic Care Management? In USA with average number of chronic cases increasing by a large number and need of chronic care management has

The healthcare industry has been rapidly evolving with the introduction of remote patient monitoring and telehealth services; they are considered to be at the forefront of transformation. Integrating these services into the healthcare industry promises a more coordinated and collaborative approach.
Patients and doctors are now working together more closely than ever before to make way for improved care coordination. In this blog, we will have a closer look at the importance of care coordination and how RPM and telehealth services are enhancing care coordination.
Before we dive deep, let’s have a discussion about the basics.
By the definition of care coordination is the process of ensuring that a patient’s healthcare journey is seamless, efficient, and effective. It involves the organized, concerted efforts of various healthcare professionals and services to provide compassionate care.
This approach is crucial, especially for patients with multiple healthcare needs, as it ensures that all aspects of their care are addressed and managed in a coordinated manner.
A key element of care coordination is communication. Effective communication between healthcare providers, patients, and sometimes their families is essential for successful care coordination. It involves sharing patient information, treatment plans, and updates among all parties involved in a patient’s care. This ongoing dialogue helps in making well-informed decisions and avoiding unnecessary duplications in treatment.
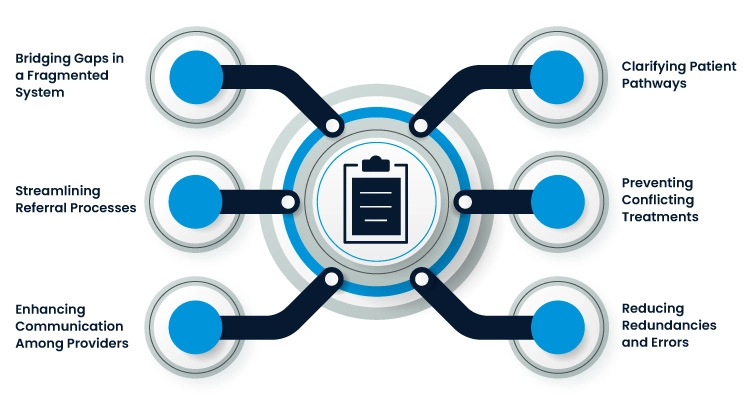
Care coordination is considered important due to specific reasons:
The US healthcare system often suffers from fragmentation across primary, emergency, and specialty care. Care coordination plays a crucial role in bridging these gaps and unifying differing processes, ensuring a more streamlined and cohesive healthcare experience.
Care coordination simplifies the often complex referral process. It eliminates the need for referral staff to navigate through cumbersome processes and extensive lists, thereby increasing the efficiency and timeliness of patient care.
Effective care coordination ensures specialists receive comprehensive information about the patient’s history and the reasons for referral. It also keeps primary care physicians updated about the outcomes of specialist consultations, promoting better-informed care decisions.
Patients often face confusion regarding referrals, appointment scheduling, and follow-up care. Coordinated care helps demystify these processes, providing clear guidance to patients as they navigate between primary care and specialists.
With care coordination, the risk of conflicting treatments prescribed by different providers is significantly reduced. This proactive approach helps avoid adverse health outcomes that can arise from incompatible medications or treatment plans.
Remote Patient Monitoring (RPM) represents a significant stride in healthcare innovation, particularly in enhancing care coordination. This technology transcends traditional care boundaries, offering a comprehensive approach to patient monitoring outside clinical settings.
RPM goes beyond standard health tracking; it’s a sophisticated system that captures and transmits a wide array of patient health data, including blood pressure, glucose levels, and oxygen saturation. By enabling patients to participate actively in their health monitoring, RPM fosters a deeper connection between patients and their care providers.
The real-time data provided by RPM devices allows healthcare providers to make timely, informed decisions. This immediacy is especially crucial for patients with chronic conditions, as it enables swift interventions in response to concerning health indicators, thus preventing potential emergencies.
Telehealth and RPM incorporate various digital communication tools, enhancing the interaction between patients and healthcare providers. These platforms range from video consultations to secure messaging systems, providing versatile options for ongoing health discussions and assessments.
RPM platforms often include educational resources tailored to patients’ specific health conditions. This feature not only informs patients about their health but also equips them with the knowledge to manage their conditions proactively. Moreover, features like medication reminders help patients adhere to their treatment regimens, contributing to better health outcomes.
Effective care coordination and Telehealth services significantly increase patients’ access to healthcare. Patients in remote or underserved areas, who previously had limited access to specialist care, can now consult with healthcare professionals via Telehealth platforms. This reduces the need for long-distance travel and ensures timely medical attention.
Consider a patient, Maria, who has been diagnosed with Type 2 diabetes. Maria lives in a rural area, far from her primary care physician and endocrinologist. Maria’s healthcare team utilizes Telehealth services to conduct virtual consultations. Through RPM, her daily glucose levels and dietary habits are monitored remotely.
Maria’s primary care doctor, endocrinologist, and nutritionist collaborate to analyze her health data, communicated through a shared EHR system. They work together to adjust her medication, diet, and exercise plan.
As a result, Maria experiences better management of her diabetes. Her glucose levels become more stable, and she gains a better understanding of her condition. She also saves time and money by reducing physical clinic visits.
The integration of Remote Patient Monitoring (RPM) and Telehealth services into healthcare systems marks a revolutionary step in enhancing care coordination. These technologies bridge the gap between patients and healthcare providers, offering a more personalized, efficient, and accessible healthcare experience.
This evolution in healthcare is not just about embracing new technologies; it’s about fundamentally transforming the patient-care provider relationship, ensuring that each patient’s journey through the healthcare system is as smooth and effective as possible.
As we continue to innovate and integrate these services, the future of healthcare looks more promising, patient-centered, and coordinated than ever before.

What is Chronic Care Management? In USA with average number of chronic cases increasing by a large number and need of chronic care management has

Telehealth Vs Telemedicine: Are They Both Same? In the wake of the COVID-19 pandemic, healthcare providers have witnessed a significant shift in patient care delivery,
Talk to an Expert Now