

Ever since the reform made by CMS in care models, one phrase that you may have heard is value-based care. This concept has not just been a buzzword but a pivotal shift in our approach to patient care.
You might be pondering the rationale behind CMS’s reforms and the essence of what is value-based care. This blog aims to demystify these changes and explore how this shift impacts not only our patients but also our daily clinical practices.
Read it till last as we are going to explore the multifaceted aspects of value-based care and understand its role in guiding us toward a more responsive and patient-oriented healthcare environment.
Value-based care is a transformative approach that flips the traditional healthcare script. Instead of the conventional fee-for-service model, where healthcare providers are reimbursed based on the quantity of care delivered, Value-Based Care shifts the focus to the quality of care provided to patients.
Think of it as a paradigm shift, where patient outcomes take the center stage. It’s about ensuring that patients receive the right care, at the right time, without unnecessary duplication of services or medical errors.
In this model, healthcare providers are rewarded for helping patients improve their health, reduce the incidence and impact of chronic disease, and live healthier lives in an evidence-based way.
Adapting to Value-Based Care is not just a strategic move—it’s a crucial pivot for the future of healthcare. But why does this shift hold such paramount importance, and why should you, as a healthcare provider, embrace it? Let’s unfold the reasons.
So, why adapt to Value-Based Care? Because it represents the future of patient-centered healthcare. It’s a journey towards more meaningful, outcome-oriented care that resonates with the needs of our patients and the broader goals of the healthcare community.
When we shift the lens to view healthcare through the eyes of our patients, Value-Based Healthcare takes on a new dimension. It’s more than a model; it’s a promise of a more engaged, personalized, and effective healthcare journey.
For patients, this means their involvement and experiences are not just valued—they are pivotal in shaping their health outcomes. Let’s understand it through an example:
A patient with diabetes. In a traditional healthcare model, patient’s treatment might focus solely on managing her symptoms. However, under Value-Based Healthcare, The journey is different healthcare team is incentivized to engage patient in his treatment plan actively.
They work with her to manage her condition proactively, incorporating lifestyle changes, regular monitoring, and personalized adjustments to her treatment. The result? The patient not only experiences better control of her diabetes but also improves her overall health and quality of life.
This model is centered around patient engagement, recognizing that informed and involved patients are more likely to follow through with treatments, make healthier lifestyle choices, and proactively manage their health.
Some of the key Value-Based Care Models that are shaping the future of healthcare:
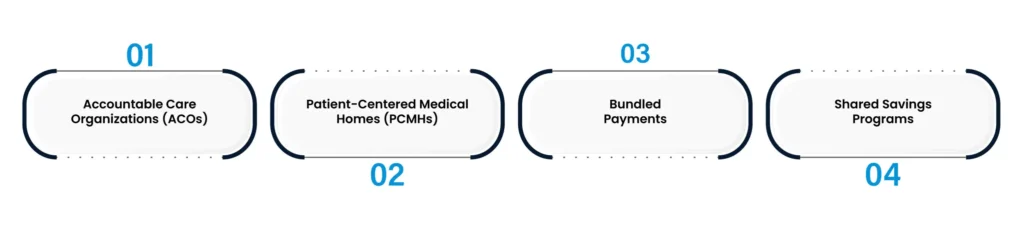
These are groups of doctors, hospitals, and other healthcare providers who come together voluntarily to provide coordinated high-quality care to their Medicare patients. The aim is to ensure that patients, especially those with chronic illnesses, get the right care at the right time while avoiding unnecessary duplication of services and preventing medical errors.
PCMHs focus on primary care that is patient-centered, comprehensive, team-based, coordinated, accessible, and committed to quality and safety. This model encourages primary care practices to develop deeper relationships with patients and provide coordinated care, improving health outcomes and patient experience.
Under this model, providers receive a single bundled payment for all the services a patient receives during a treatment episode or over a specified period. This encourages providers to offer cost-effective care, as they must manage resources wisely to stay within the budget while maintaining or improving quality standards.
In these programs, providers are rewarded for reducing healthcare costs while meeting standards for high-quality care. If providers keep their patient costs below a predefined benchmark while meeting quality thresholds, they share in the savings achieved.
The Value-Based Care model hinges on performance-based payment systems. Essentially, healthcare providers are reimbursed based on the quality of care they deliver, not just the quantity. CMS evaluates healthcare providers on several key metrics to ensure that patient care is effective, efficient, and aligned with specific health outcomes. These metrics fall into various categories, including quality of care, patient experience, and healthcare utilization.
Let’s delve deeper into these metrics:
Quality of Care: This includes measures like infection rates, readmission rates, and other clinical indicators that reflect the effectiveness of care. Providers are assessed on how well they manage chronic diseases, prevent hospital-acquired conditions, and maintain high standards of clinical performance.
Patient Experience: This involves evaluating patient satisfaction and engagement. Measures such as patient feedback on the care received, the level of communication and understanding between patient and provider, and overall patient engagement in their care process are crucial.
Healthcare Utilization: This looks at the efficiency of care delivery, focusing on the appropriate use of medical resources. Metrics include the number of unnecessary tests or procedures avoided, effective coordination of care among different providers, and reduction in avoidable hospital admissions and emergency room visits.
Under this model, healthcare providers are encouraged to adopt practices that prioritize patient outcomes and cost-effectiveness. This includes leveraging technology for better data analysis and patient management, adopting evidence-based practices, and focusing on preventive care to reduce the likelihood of costly interventions later.
Value-Based Care, a significant shift from traditional healthcare models, brings with it a multitude of benefits that resonate across the healthcare spectrum – from patients to providers, and even to the healthcare system as a whole.
Improved Patient Outcomes: At the core of Value-Based Care is the commitment to patient health and well-being. This model emphasizes preventive care, early intervention, and continuous management of chronic conditions, leading to better health outcomes for patients. With a focus on quality over quantity, patients receive more effective and personalized care.
Enhanced Patient Experience: Value-Based Care models prioritize patient-centered services, which means healthcare delivery is more attuned to the needs and preferences of patients. This approach fosters better patient-provider relationships, higher patient satisfaction, and improved overall experience with the healthcare system.
Reduced Healthcare Costs: By focusing on preventive care and efficient management of chronic diseases, Value-Based Care helps reduce hospital readmissions and unnecessary medical procedures, which in turn leads to a reduction in healthcare spending. This cost-effectiveness is beneficial not only for patients but also for providers and payers.
Increased Provider Satisfaction: Healthcare providers under Value-Based Care models often experience greater job satisfaction. This is due to the emphasis on quality care, better patient outcomes, and reduced pressure of high patient volumes. Providers have the opportunity to engage more meaningfully with their patients, leading to a more fulfilling professional experience.
Promotion of Healthcare Innovation: This model encourages the adoption of new healthcare technologies and practices, such as telehealth, electronic health records (EHR), and personalized medicine. Providers are motivated to innovate and improve care delivery, contributing to the advancement of the healthcare industry.
Alignment with Public Health Goals: Value-based care aligns closely with broader public health objectives, such as improving population health, addressing health disparities, and promoting a healthier society. By focusing on outcomes and preventive care, this model contributes to healthier communities and a stronger public health infrastructure.
Hospital VBP fundamentally transforms the way hospitals are reimbursed. Instead of solely relying on the traditional fee-for-service model, this program adjusts payments to hospitals based on the quality of care they deliver. The idea is straightforward yet powerful: reward hospitals for providing high-quality, patient-centered care, and reduce payments for those that don’t meet these standards.
The performance of hospitals under the VBP program is evaluated based on several key measures, categorized into different domains:
Through these measures, Hospital VBP encourages hospitals to continuously evaluate and improve their performance in delivering quality care. The goal is to create an environment where hospitals are not just health care providers but are actively engaged in enhancing patient outcomes, improving safety, and reducing costs.
In conclusion, the shift towards Value-Based Care represents a monumental change in the landscape of healthcare. It’s a change that brings the focus back to what truly matters in healthcare: quality, efficiency, and, most importantly, patient outcomes.
This model isn’t just about transforming payment structures or healthcare practices; it’s about reshaping our entire approach to healthcare delivery. As we embrace these changes, we stand on the cusp of a new era in healthcare – one that promises better care for patients, more satisfaction for providers, and a more sustainable system for all.
Talk to an Expert Now